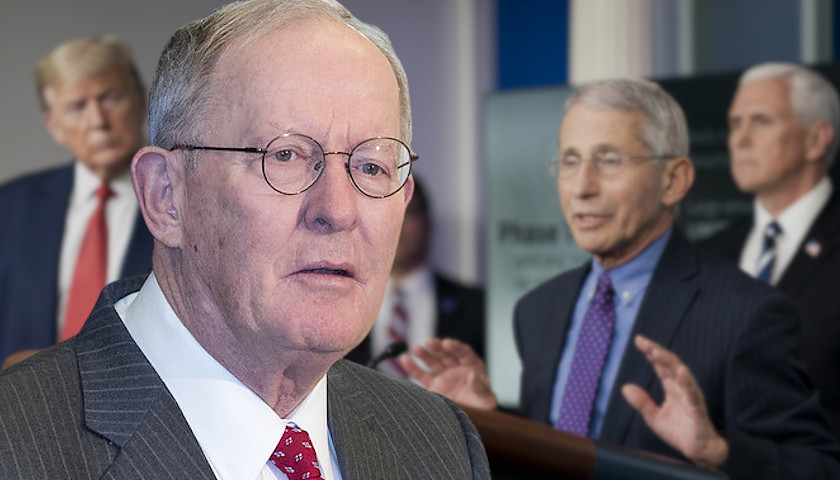
Over the weekend, Senator Lamar Alexander (R-TN) told Mayor Jill Holland of McKenzie, Tennessee that he will encourage Senator Orrin Hatch (R-UT) to conduct hearings at the Senate Finance Committee he chairs on whether an Obama-era regulation that is hitting West Tennesssee’s Dr. Bryan Merrick should be revoked, along with other corrections.
A spokesperson for the senator confirmed to The Tennessee Star that Alexander will ask Hatch to hold those hearings.
Alexander chairs the Senate Health, Education, Labor, and Pensions (HELP) Committee, which he says does not have jurisdiction over the CMS regulation. Senator Hatch chairs the Senate Finance Committee, which does have jurisdiction over the CMS regulation.
Surprising as that may seem, official Senate rules confirm that the Senate Finance Committee has jurisdiction over all health programs based on federal taxes, which includes Medicare and Medicaid.
Senator Paul Toomey (R-PA) chairs the Health Care Subcommittee of the Senate Finance Committee, the most likely place for such hearings to be held.
On Friday, Mayor Jill Holland of McKenzie sent a letter to Senator Alexander asking him to hold hearings of the Senate HELP committee he chairs for the purpose of revoking the CMS regulation, as The Star reported:
Writing “on behalf of the citizens of Northwest Tennessee,” Mayor Jill Holland asked Alexander, “as Chairman of the Senate Health, Education, Labor, and Pensions Committee [to] schedule, at the earliest opportunity, a hearing of the appropriate subcommittee to consider the revocation or modification of a particularly egregious Obama-Era regulation promulgated by the Centers for Medicare and Medicaid Services (CMS) in December, 2014, “Medicare Program; Requirements for the Medicare Incentive Reward Program and Provider Enrollment; Final Rule.”
“This regulation, and its abusive implementation by CMS, is now jeopardizing the health care of hundreds of eventually thousands of citizens in and around McKenzie, Tennessee, our city of 5,000 residents in Carroll, Henry, and Weakley counties,” Holland wrote.
One day earlier, on Thursday, Alexander met briefly with Dr. Merrick and one of his attorneys, former State Senator Roy Herron (D-Dresden) on Capitol Hill in Washington on Thursday.
Merrick and Herron were just coming out of a scheduled meeting with Alexander’s Chief of Staff to ask for help in the case in which the West Tennessee doctor has been victimized by an Obama-era regulation with regards to Medicare billing that has been abused by the Centers for Medicare and Medicaid Services (CMS).
The hallway meeting with Alexander lasted for about five minutes Herron told The Star.
As The Star reported previously, CMS has abruptly terminated the Medicare billing privileges of Dr. Merrick, one of the owners of the McKenzie Medical Center, located in the small West Tennessee city of McKenzie, over $670 in billing errors, citing the regulation finalized by the CMS in December 2014 over the objections of several physicians group that warned its vagueness would certainly lead to the types of bureaucratic abuses that have deprived Dr. Merrick of his due process rights and also harmed the hundreds of West Tennessee residents who depend on him and his clinic for their health care needs.
“Sen. Alexander and his staff have been in touch with Dr. Merrick since we first learned of the situation in early September. At Dr. Merrick’s request, we have discussed Dr. Merrick’s case with the Centers for Medicare and Medicaid Services numerous times. Every possible step, except those prohibited by the Senate Rules and ethics guidance, has been taken to help Dr. Merrick and his patients. Dr. Merrick has appealed the Centers for Medicare and Medicaid Services’ decision and his appeal will be heard by an administrative law judge,” a spokesperson for Senator Alexander told The Star.
According to Alexander’s staff Senator Alexander is constrained by rules that restrict their interference with specific cases once they are in the enforcement process. They acknowledged that a review of the rules and procedures for dealing with fraud in billing and delivery of medical treatment is appropriate to insure that the legitimate and necessary intent to protect taxpayers’ interests by dramatically reducing fraud, waste and abuse in the Medicare and Medicaid system doesn’t produce overreach or abuse of those who simply make mistakes or coding errors.
Merrick is not the only doctor who has been ensnared by the bureaucratic abuses of CMS in implementing this vague Obama-Era regulation and related Medicare regulations, regulation commentary, and sub-regulatory policies and guidelines.
“During 2015, more than 1.2 million non-institutional health care providers participated in the Medicare program. Over the last year, a number of these providers have unexpectedly found themselves in a difficult situation where their Medicare number has been either ‘deactivated’ or ‘revoked.’ While Medicare deactivation actions remain somewhat rare, over the past year, the number of Medicare revocation actions taken by Medicare Administrative Contractors (MACs) appears to have greatly increased,” attorney Robert Liles, managing partner at Liles Parker, a boutique health care law firm with offices in Washington, D.C. and Houston, Texas, wrote in August 2016.
Since then, the number of Medicare revocation actions by CMS has continued to accelerate, Liles told The Star in an exclusive interview on Monday.
His firm deals with many similar cases to Dr. Merrick’s in which Medicare billing privileges have been revoked due to administrative or clerical errors, with devastating consequences for the doctors as well as their patients, Liles added.
“I know of numerous cases where a doctor moved their office and either the office administrator didn’t get in the online system properly or some other administrative error was made, and the contractor [who handles billing review for CMS] swears they never got it,” Liles said, and as a result the doctor’s Medicare billing privileges were revoked.
“I also know of circumstances where the contractors go by small home health care agencies at lunch time, when the offices are closed, and revoke their Medicare billing privileges,” Liles noted.
“I have three physician clients, all in the Houston area, one in palliative care, one in post acute care, and one in wound care. All three had their Medicare billing privileges revoked because the Medicare contractor conducted a site visit, and went to the wrong site due to clerical errors,” attorney Jennifer Papapanagiotou told The Star.
“The problem is the current CMS system takes an administrative error by a doctor and punishes them by revoking their Medicare billing privileges for three years,” Papapanagiotou added.
For physicians with practices that are predominantly with elderly patients whose health care is provided by Medicare, that three year gap in revenue often puts them out of business. It also is very destructive for the health care of their patients.
“There are just a handful of wound doctors in Houston,” Papapanagiotou said. When CMS revoked the Medicare billing privileges of one of those wound doctors, it disrupts the ability of many wound care patients, most elderly, from receiving care.
“The appeal process is so weighted in favor of CMS,” Papapanagiotou added. As a result, very few appeals of Medicare billing privileges by physicians succeed, not because they have done anything wrong from a medical care or business perspective, but because of innocent or inadvertent clerical errors.
“Here’s the problem,” attorney Liles told The Star.
“It goes to a fundamental error in the way this Medicare health care system is set up. This massive agency at CMS is run by just 5,000 federal employees. The way they run the program is they contract out almost all the actual work to private companies. It’s the private companies that go out in the field to do the audits,” Liles said.
“These private companies receive hundreds of millions of dollars in revenue from CMS. The only way they keep getting paid is by finding fault with the doctors. So that’s what they do. We should not be contracting out program integrity functions [from CMS employees to these private companies,” Liles concluded.
Papapanagiotou told The Star she has been asked to represent numerous physicians who have had their Medicare billing privileges revoked because they billed deceased patients, a circumstance similar to Dr. Merrick’s case.
“If a provider makes more than three errors in billing for a deceased beneficiary, CMS can revoke their Medicare billing privileges,” Papapanagiotou added, even if the billing errors were inadvertent or clerical errors, the billings were never paid, and the amounts involved are small.
“The ‘at least three billing errors’ interpretation by CMS that has been used by the Administrative Law Judges to sustain revocations where a physician has billed for a deceased beneficiary comes from the June 27, 2008 final rule that promulgated a number of changes to the Medicare provider enrollment regulations,” Papapanagiotou continued.
But, Papapanagiotou noted, the “at least three billing errors” interpretation by CMS is based not on the actual rule, but instead the commentary on the rule by CMS, as can be seen here in this link.
Such commentaries carry lesser weight if an appeal ever went to the final step of federal litigation, but Adminstrative Law Judges who rule on earlier steps in the appeal process, have very little leeway in making their decisions, and apparently rely on commentaries as much as they do the finalized regulation.
Merrick’s Medicare billing privileges, however, were revoked based on the 2014 Obama-era regulation, though apparently the “three billing errors for deceased beneficiaries” standard was also applied.
An even more direct route to end this abuse is available however.
President Trump has the authority to instruct CMS to initiate the rule making process to revoke the rule.
During that rule making process, CMS is required to solicit public comments on the rule and whether it should be revoked.
At the completion of that process–which could take anywhere from 90 days to a year–CMS could revoke the rule.
Sources tell The Star that efforts are currently under way to bring the matter directly to President Trump’s attention, and request him to provide that specific instruction to CMS.
“While this particular case is working its way through the review process, which should be expedited, there is no reason to delay having hearings and getting answers from the CMS Director Seems Verma about ways to protect taxpayer dollars while also insuring that nameless, faceless bureaucrats can’t use to the rules and procedures to abuse those who are trying to honestly comply with the complexities of the Medicare and Medicaid billing systems,” said conservative political strategist Steve Gill.
“Those who commit fraud and intentionally soak the taxpayers should be identified and prosecuted. But we have given too much opportunity for too long to government agencies and bureaucrats to selectively enforce the law as a weapon against people with good intentions; draining the swamp should include focusing on reducing the unbridled and overreaching powers of government bureaucrats,” Gill added.




[…] this month, Alexander called on Senator Orrin Hatch (R-UT) to hold hearings in the Senate Finance Commmittee he chairs on the […]
[…] last month, Senator Lamar Alexander (R-TN) called on Senator Orrin Hatch (R-UT) to hold hearings at the Senate Finance Committee he chairs to consider revoking the […]
[…] Monday, The Star reported that Senator Lamar Alexander (R-TN) has asked Senator Orrin Hatch (R-UT) to hold hearings of the […]
I have worked years in Medicare compliance and realize that many physicians do not put the processes in place to make sure they are in billing compliance. I do not understand how someone could manage to bill for a deceased patient unless they were running a sloppy billing operation, or attempting to commit fraud. I really do not have a lot of sympathy for this physician.
Mistakes are made everywhere. It would be real easy to type the wrong Medicare ID number. This should be considered along with any other problems the doctor has had with billing.